Retinol-Binding Protein (RBP)
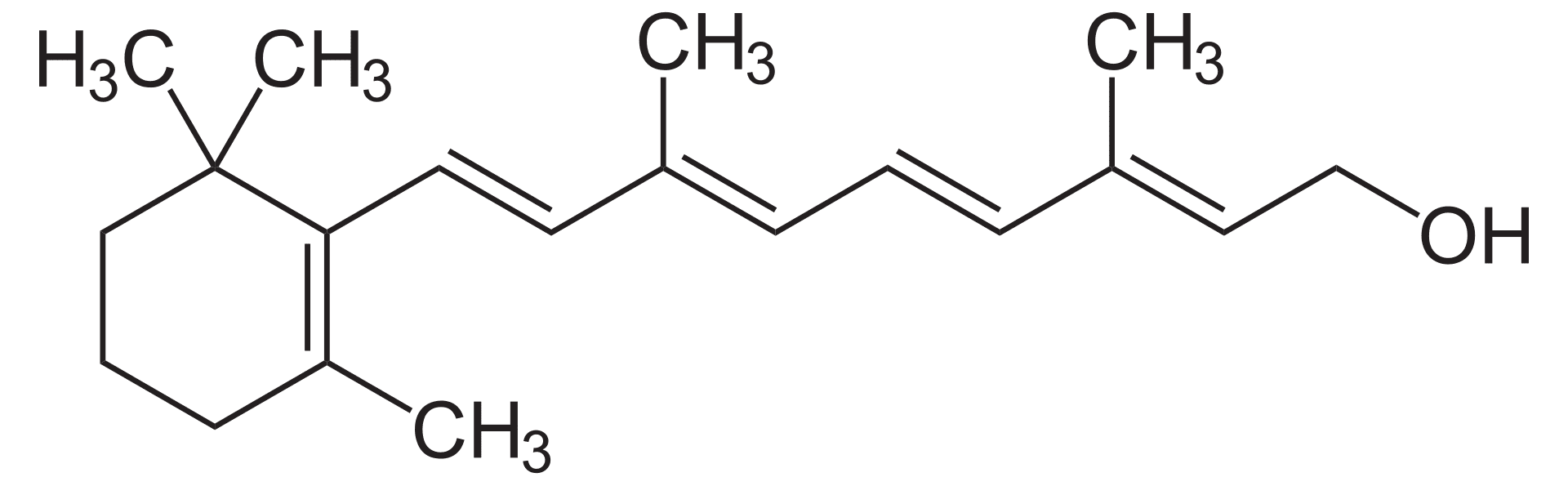
 Vitamin A is a fat-soluble vitamin essential for numerous biological functions, including vision, immune function, and cell growth. However, its hydrophobic nature makes it difficult to transport through the aqueous environment of the bloodstream. This is where retinol-binding protein (RBP) comes into play.
Vitamin A is a fat-soluble vitamin essential for numerous biological functions, including vision, immune function, and cell growth. However, its hydrophobic nature makes it difficult to transport through the aqueous environment of the bloodstream. This is where retinol-binding protein (RBP) comes into play.
The Role of RBP in Vitamin A Transport
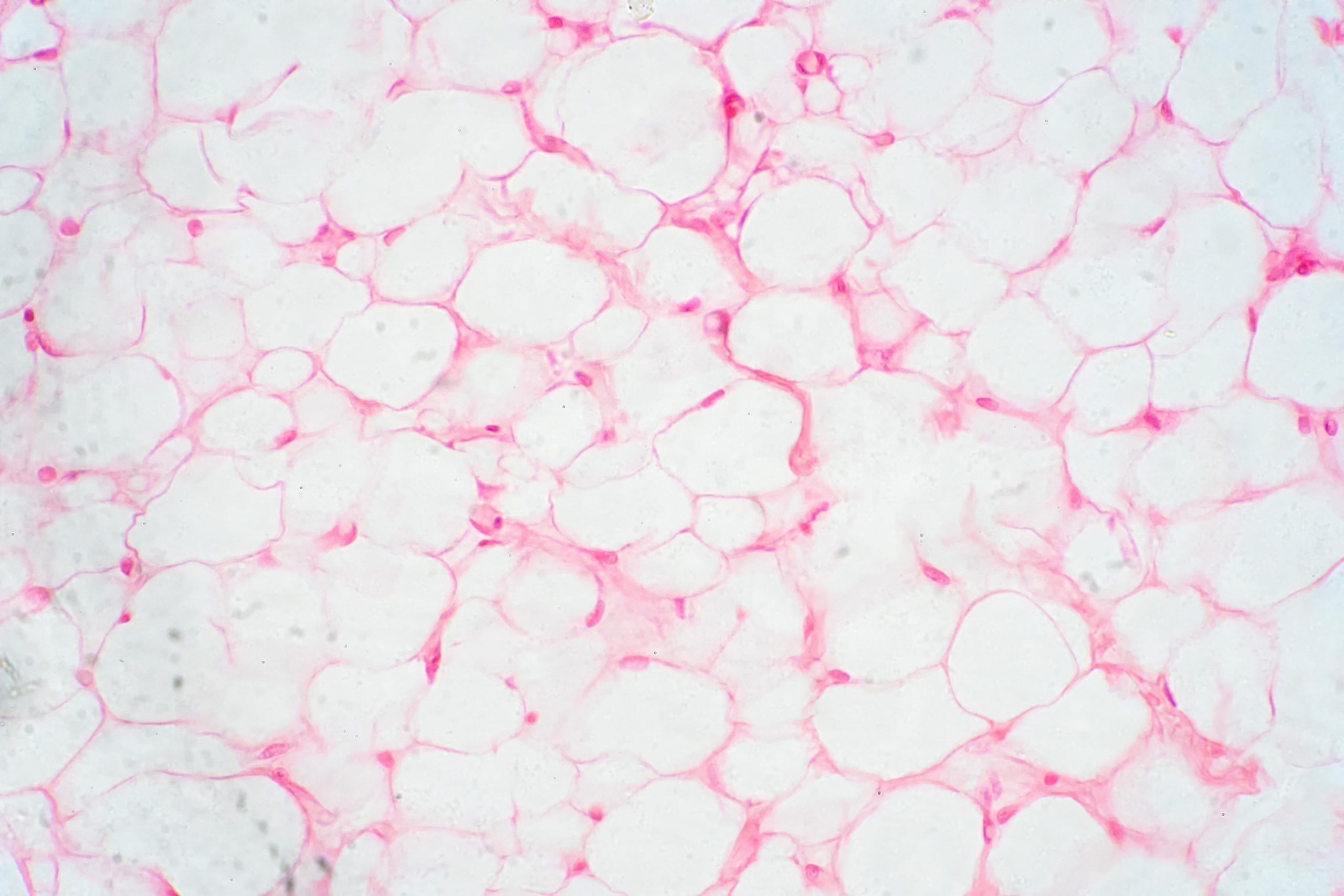
RBP is a small protein that plays a vital role in vitamin A transport. It binds specifically to retinol, the alcohol form of vitamin A. This binding is essential for several reasons: first, it increases the solubility of retinol in the blood, preventing its aggregation and potential toxicity; second, it protects retinol from degradation, ensuring its safe delivery to target tissues; and third, it helps maintain appropriate levels of vitamin A in the blood, preventing both deficiency and excess.
The RBP-Transthyretin Complex
The stability and longevity of the RBP complex in the bloodstream is significantly enhanced by its interaction with transthyretin (previously known as prealbumin). This protein acts as a chaperone, forming a stable ternary complex with RBP and retinol. Transthyretin prevents renal filtration by binding to RBP, which physically shields it from the filtration process in the kidneys. This prevents RBP from being prematurely eliminated from the body, prolonging its circulation time and ensuring a more sustained delivery of vitamin A to target tissues.
By preventing renal filtration, transthyretin effectively extends the half-life of RBP in the plasma. This means that RBP remains in the bloodstream for a longer period, allowing for a more gradual and sustained release of retinol to tissues as needed.
The RBP-transthyretin complex provides a stable and protected environment for retinol, safeguarding it from degradation and ensuring its efficient delivery to various tissues throughout the body. This is particularly important for tissues that have a high demand for vitamin A, such as the retina, epithelial cells, and immune cells.
Metabolism and Regulation of RBP
RBP is a crucial molecule involved in the transport and regulation of vitamin A. Its production and levels are tightly controlled to ensure optimal vitamin A delivery to tissues and prevent both deficiency and excess. RBP is primarily synthesized in the liver, which acts as the primary production site. The liver responds to the body’s demand for vitamin A by adjusting RBP synthesis accordingly. When vitamin A intake increases, the liver may produce more RBP to accommodate the increased supply. Conversely, a decrease in vitamin A intake can lead to reduced RBP production.
In addition to vitamin A intake, liver function plays a crucial role in RBP regulation. Liver diseases or disorders that impair liver function can affect RBP production, leading to abnormal levels. For example, conditions such as cirrhosis or hepatitis can reduce RBP synthesis, potentially contributing to vitamin A deficiency.
Furthermore, kidney health also influences RBP metabolism. The kidneys play a role in the clearance of RBP from the bloodstream. Kidney diseases or disorders that impair renal function can disrupt the balance between RBP production and elimination, leading to altered RBP levels.
Disturbances in RBP levels can have significant health implications. Low RBP levels can be a sign of vitamin A deficiency, which can lead to various symptoms such as night blindness, dry eyes, impaired immune function, and increased susceptibility to infections. On the other hand, excessively high RBP levels can indicate vitamin A toxicity, which can cause symptoms like headache, nausea, vomiting, and liver damage.
Clinical Significance of RBP
Measuring RBP levels can be a valuable diagnostic tool in assessing both nutritional status and organ function. RBP is a sensitive indicator of vitamin A status, as its levels are directly influenced by vitamin A intake and metabolism.
Low RBP levels can be a strong indicator of vitamin A deficiency. This is because RBP is primarily synthesized in response to adequate vitamin A availability. When vitamin A intake is insufficient, RBP production may decrease, leading to lower levels in the blood. Vitamin A deficiency can have serious consequences, including night blindness, dry eyes, impaired immune function, and increased susceptibility to infections.
Elevated RBP levels can suggest underlying health issues, particularly those involving the liver or kidneys. Liver diseases, such as cirrhosis or hepatitis, can impair RBP synthesis or clearance, leading to increased RBP levels. Additionally, certain kidney diseases can also affect RBP metabolism, resulting in elevated levels.
By measuring RBP levels, healthcare providers can assess the body’s vitamin A status and identify potential nutritional deficiencies or underlying medical conditions. RBP measurements can be particularly useful in individuals at risk of vitamin A deficiency, such as those with malabsorption disorders, chronic diseases, or poor dietary intake.
Closing Thoughts
Retinol-binding protein (RBP) plays a critical role in the transport and regulation of vitamin A, a vital nutrient for human health. By binding retinol and facilitating its transport in the bloodstream, RBP ensures that this essential vitamin reaches the tissues where it is needed.
The interaction between RBP and transthyretin enhances the stability and longevity of the retinol-RBP complex, ensuring efficient delivery of vitamin A to target cells. The tight regulation of RBP levels by factors such as vitamin A intake, liver function, and kidney health reflects the importance of maintaining adequate vitamin A status.
Measuring RBP levels can be a valuable diagnostic tool for assessing nutritional status and identifying potential health issues related to vitamin A metabolism. By understanding the role of RBP in vitamin A transport and regulation, healthcare professionals can better diagnose and treat conditions associated with vitamin A deficiency or toxicity.
Matthew A. Webster, MA, MS, ED.D, LPC
Dr. Matt Webster is a professional educator, nutritionist, and therapist located in the Houston, Texas area. He specializes in couples therapy, sexuality, and maladaptive eating patterns with a focus on the role of nutrition. More About Matt >>
Last modified: