Vitamin K – Counterbalance to Anticoagulant Therapy
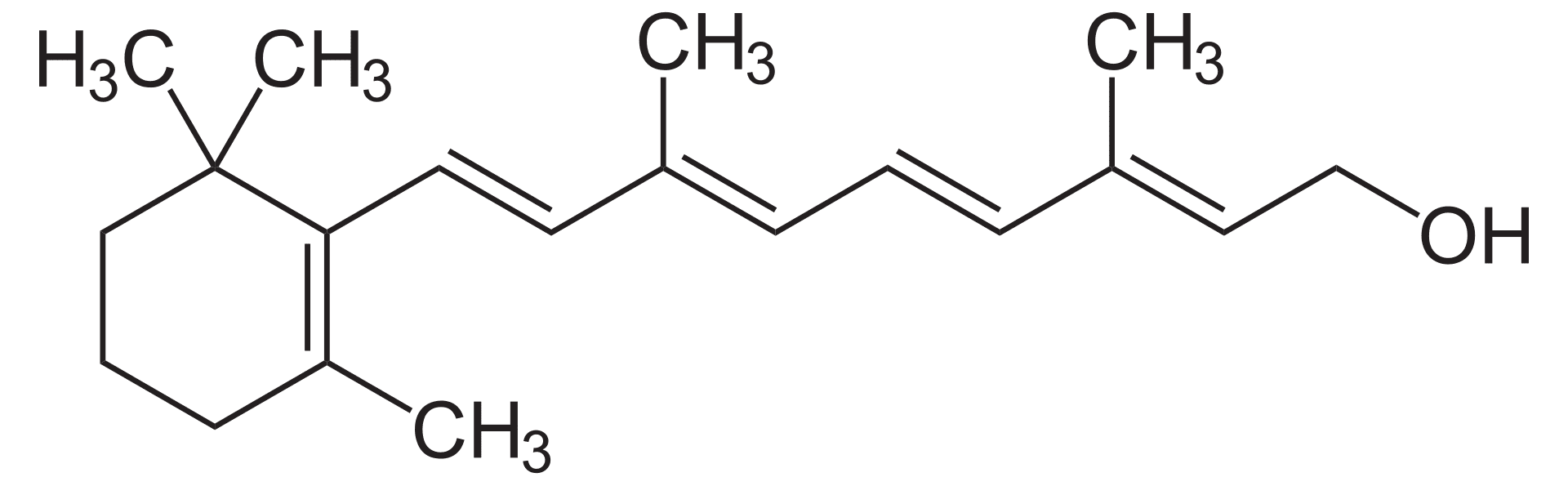
 Vitamin K is a fat-soluble vitamin essential for various bodily functions and is frequently administered to patients undergoing extensive anticoagulant therapy. This practice is rooted in the intricate relationship between Vitamin K and blood clotting, as well as the specific actions of anticoagulant medications.
Vitamin K is a fat-soluble vitamin essential for various bodily functions and is frequently administered to patients undergoing extensive anticoagulant therapy. This practice is rooted in the intricate relationship between Vitamin K and blood clotting, as well as the specific actions of anticoagulant medications.
The Mechanism of Anticoagulants
Anticoagulants like warfarin, are prescribed to prevent the formation of blood clots. These medications work by disrupting the intricate process by which blood clots form. This process involves a cascade of events that culminates in the formation of a fibrin clot, which is a protein mesh that traps blood cells and platelets. At the heart of this is a series of proteins known as clotting factors that are produced by the liver and require Vitamin K as a cofactor for their activation. Vitamin K acts as a catalyst, enabling these clotting factors to function properly.
When anticoagulants like warfarin are introduced into the body, they interfere with the body’s ability to utilize Vitamin K. This interference can occur in several ways. Warfarin can bind to Vitamin K, preventing it from interacting with the clotting factors, and warfarin can inhibit the enzyme that recycles Vitamin K, reducing its availability in the body.
By limiting the availability of Vitamin K, anticoagulants effectively disrupt the clotting cascade. This disruption prevents the activation of clotting factors, thereby inhibiting the formation of blood clots. This mechanism is particularly important in individuals at risk of blood clots, such as those with atrial fibrillation, deep vein thrombosis, or pulmonary embolism.
The Importance of Vitamin K in Blood Clotting
Vitamin K plays a pivotal role in the intricate process of blood clotting. It acts as a cofactor, a substance that is necessary for the proper functioning of certain enzymes involved in the clotting cascade. These enzymes are responsible for activating a series of proteins known as clotting factors, which are essential for the formation of blood clots. When a blood vessel is injured, platelets gather at the site of the wound and release substances that initiate the clotting process. These substances trigger a cascade of reactions involving the clotting factors. Vitamin K is crucial for the activation of several key clotting factors, including Factors II, VII, IX, and X.
Without sufficient Vitamin K, these clotting factors cannot function optimally. As a result, the blood clotting process becomes impaired. This can lead to excessive bleeding, even in response to minor injuries. In severe cases of Vitamin K deficiency, spontaneous bleeding may occur. Maintaining adequate Vitamin K levels is essential for preventing excessive bleeding and ensuring proper hemostasis, the body’s ability to stop bleeding.
Counteracting Anticoagulant Overdose or Bleeding Risk
In instances of warfarin overdose or excessive bleeding associated with prolonged anticoagulant therapy, Vitamin K is administered as a corrective measure. Warfarin, as a blood thinner, works by inhibiting the activity of Vitamin K. By reducing Vitamin K’s availability, warfarin prevents the activation of clotting factors, thereby reducing the body’s ability to form blood clots.
When a warfarin overdose occurs or when excessive bleeding arises, it indicates that the anticoagulant’s effect has become too pronounced. In such situations, administering Vitamin K can help to counteract the anticoagulant’s action. By replenishing Vitamin K levels, the body can resume the production of clotting factors more effectively. This restoration of clotting factor levels is essential to prevent excessive bleeding and maintain hemostasis.
Impact of Anticoagulants on Gut Bacteria
While anticoagulants primarily exert their effects by directly interacting with Vitamin K, they can also indirectly influence Vitamin K levels. Certain anticoagulants, particularly those that have been used for extended periods, can disrupt the delicate balance of the gastrointestinal flora. These beneficial bacteria, which reside in the intestines, contribute to the body’s endogenous production of Vitamin K. This means that they synthesize Vitamin K within the intestines, supplementing the Vitamin K obtained from dietary sources. When the gut bacteria are disturbed by anticoagulant therapy, their ability to produce Vitamin K may be compromised. This disruption can lead to a decrease in the body’s overall Vitamin K levels, further exacerbating the risk of Vitamin K deficiency and associated bleeding complications. Being aware of the indirect effects of anticoagulants on Vitamin K levels is essential for the effective management of patients receiving these medications.
Closing Thoughts
Vitamin K serves as a valuable tool in managing the balance of blood clotting risk in patients receiving anticoagulant therapy. By counteracting the effects of anticoagulants and supporting the body’s natural clotting mechanisms, Vitamin K helps to prevent both excessive bleeding and the formation of unwanted blood clots. This delicate balance is crucial for maintaining overall health and well-being in individuals who require anticoagulant treatment.
Matthew A. Webster, MA, MS, ED.D, LPC
Dr. Matt Webster is a professional educator, nutritionist, and therapist located in the Houston, Texas area. He specializes in couples therapy, sexuality, and maladaptive eating patterns with a focus on the role of nutrition. More About Matt >>
Last modified: